Insulin resistance, also known as impaired insulin sensitivity, is a condition in which cells in your body are unable to respond normally to insulin, a hormone produced by your pancreas.
Insulin helps your body use and store glucose, or sugar, as energy. People with insulin resistance have difficulty processing glucose, and this can lead to high levels of sugar in the blood. Over time, this can increase the risk of developing type 2 diabetes, heart disease and stroke.
The exact cause of insulin resistance is unknown, but it is likely related to genetic and lifestyle factors.
It can also be caused by certain medications or medical conditions, such as polycystic ovary syndrome.
Some lifestyle changes can help reduce the risk of developing the condition, including maintaining healthy weight, getting regular exercise, eating balanced diet and reducing stress levels. In some cases, medications may also be prescribed to help control blood sugar levels.
Symptoms
It is a common precursor to Type 2 diabetes and as such, may not show any visible signs and symptoms. It, however, seems to be associated with certain medical conditions, such as:
Acanthosis Nigricans
Acanthosis nigricans is a skin disorder that causes dark, velvety patches to appear on the skin. It typically occurs in the neck, armpits, groin and other body folds.
While the condition is usually harmless, it can be a sign that you may be progressing towards type 2 diabetes.
Major Depressive Disorder
According to a study, higher levels of insulin in the bloodstream, even in the absence of diabetes, is associated with an increased risk of major depressive disorder.
Polycystic Ovary Syndrome
Research shows that PCOS is linked to insulin resistance because of the hormonal imbalances, as well as lifestyle factors such as obesity.
Vascular Disease
A person with higher levels of insulin in his bloodstream may be more vulnerable to vascular diseases, including heart disease, even if he is not diabetic.
Symptoms During Progression from Insulin Resistance to Type 2 Diabetes
If you have already progressed to diabetes from insulin resistance, these following symptoms may show up:
Causes and Risk Factors
Research indicates that certain factors and medical conditions can lead to varying levels of insulin resistance.
Scientific evidence shows that heightened body fat, particularly around the midsection, and reduced physical activity are the two primary causes of insulin resistance.
The following are some of the most common causes and risk factors of the condition:
Just remember that because you have one or more of the risk factors listed above doesn’t mean that you will develop insulin resistance.
However, if you have any of these factors, it’s important to talk to your doctor about ways to reduce your risk.
Diagnosis
Diagnosis of insulin resistance typically involves a series of tests, particularly a fasting blood glucose test, an oral glucose tolerance test and a hemoglobin A1C test.
Fasting Blood Glucose Test
A fasting blood glucose test is a diagnostic test used to measure the amount of glucose present in the blood after an eight-hour period of fasting.
Fasting glucose level of less than 100 mg/dL is considered normal, while levels between 100 and 125 mg/dL are indicative of prediabetes. A level of 126 mg/dL or higher is considered to be diabetic.
Oral Glucose Tolerance Test
The Oral Glucose Tolerance Test (OGTT) is a medical diagnostic test used to detect diabetes and diagnose any other metabolic disorders related to glucose.
During the test, the patient consumes a special glucose solution, and then his blood sugar is tested at regular intervals over the next two hours.
Normal results of an OGTT differ depending on the laboratory, but generally a fasting blood glucose level (before drinking the solution) should be less than 100 mg/dl. Two hours after drinking the solution, the blood glucose level should be below 140 mg/dl. If the glucose level is higher than this, it could indicate prediabetes or diabetes.
A1C Test
The A1C test is a simple blood test that measures your average blood sugar level over the past three months. The test measure the amount of hemoglobin in the red blood cells that has been exposed to glucose over time.
A normal A1C level is between 4 and 5.7%. An A1C level of 6.5% or greater is considered to be an indication of diabetes.
Treatment and Management
The best way to do treat your insulin resistance is to improve your lifestyle.
First, it’s important to maintain a healthy diet. Eating a balanced diet that is low in processed and refined carbohydrates can help.
Also eating a balanced diet full of whole grains, fresh fruits and vegetables, lean proteins and healthy fats can help regulate your blood sugar levels and reduce your risk of insulin resistance.
Eating foods high in fiber can help keep your blood sugar levels stable.
Regular exercise can also help prevent insulin resistance by improving your body’s ability to use insulin. Aim for at least 30 minutes of moderate to vigorous physical activity every day.
It’s important to maintain a healthy weight and see your doctor regularly for check-ups to ensure that your blood sugar levels are under control.
Finally, it’s important to make sure you’re getting enough sleep. Lack of sleep can lead to increased insulin resistance, so make sure you get at least 7-8 hours of sleep each night.
Difference between Insulin Resistance and Insulin Sensitivity
Insulin resistance and insulin sensitivity are two terms that describe the way the body responds to insulin.
Insulin resistance occurs when the body’s cells become less sensitive to the effects of insulin, making it harder for the body to use glucose for energy. This can lead to high blood sugar levels and an increased risk of diabetes.
Insulin sensitivity, on the other hand, refers to how well the body responds to insulin. When you are insulin sensitive, your body is more responsive to insulin and is better able to use glucose for energy. This can help maintain healthy blood sugar levels and reduce the risk of diabetes.
What Foods Can Help Manage Insulin Resistance?
Eating the right foods can help you manage your insulin resistance and reduce its symptoms.
Here is a list of foods that can help:
If you have a question related to this blog post, write to us here and we will update this post with a response.
If you have any more questions, please feel free to write to us at support@nugenomics.in or call us directly at +91 9176655912
You can also visit Here to know more about how we can help you and make your life better.
Sources: Cleveland Clinic, Medical News Today, Healthline, Diabetes UK, NCBI.
 Cart is empty
Cart is empty 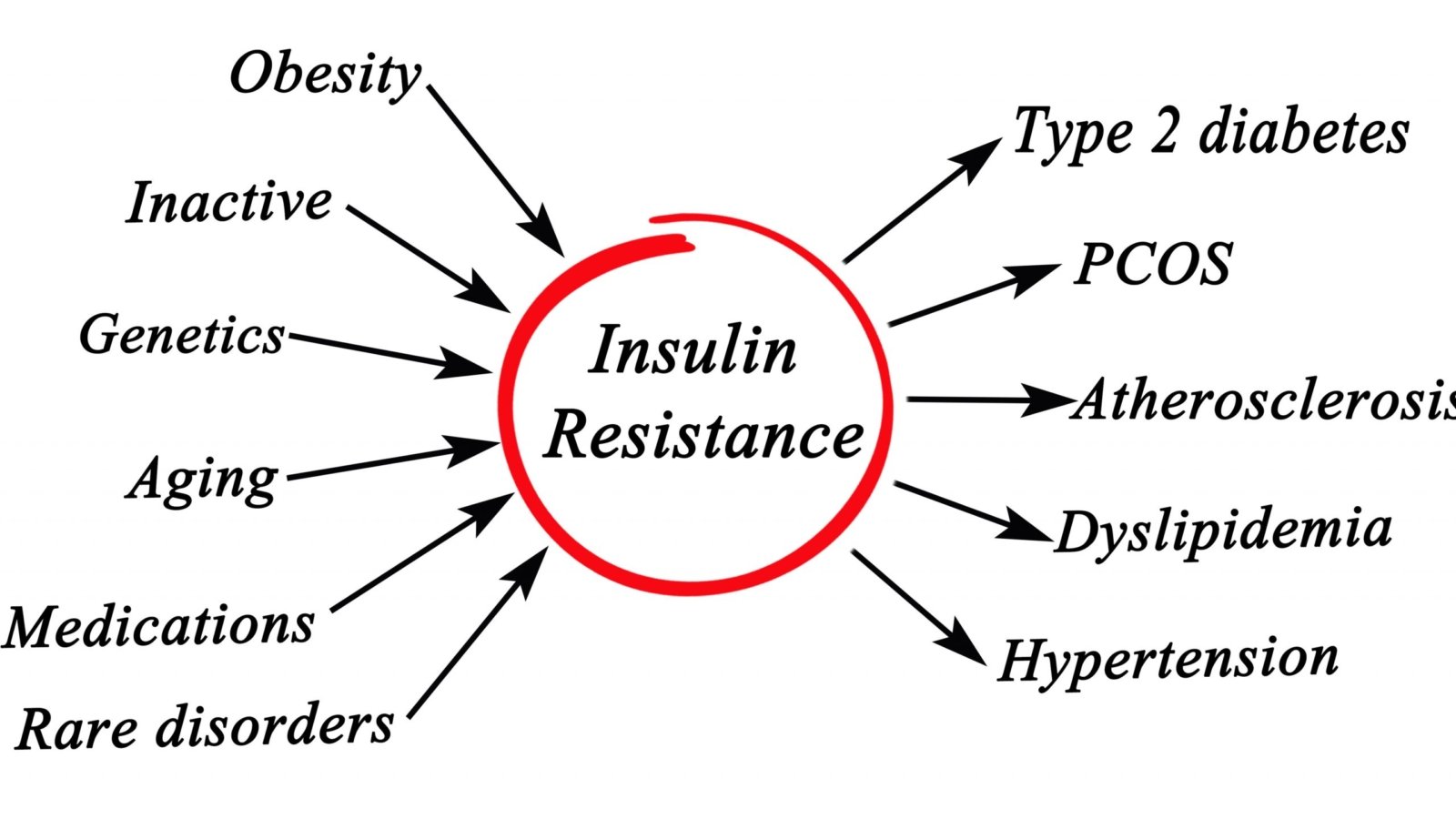
Add a Comment